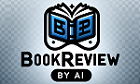
Chapter 1: Introduction
* Provides an overview of the gut-physiology syndrome (GPS), a complex condition involving interactions between the digestive system and various organs and tissues.
* Discusses the historical background and prevalence of GPS, highlighting its impact on individuals and healthcare systems.
Example: A 35-year-old woman with chronic abdominal pain, bloating, and diarrhea is diagnosed with GPS after extensive medical testing.
Chapter 2: Pathophysiology
* Explores the underlying mechanisms of GPS, including alterations in gut microbiota, immune dysfunction, and nerve signaling.
* Discusses how these abnormalities can contribute to symptoms such as abdominal pain, gastrointestinal dysfunction, and extra-intestinal manifestations.
Example: A study demonstrates that patients with GPS have a disrupted gut microbiome, characterized by decreased beneficial bacteria and increased pathogenic organisms.
Chapter 3: Diagnosis
* Presents the diagnostic criteria for GPS, emphasizing the importance of a thorough medical history, physical examination, and laboratory testing.
* Discusses the challenges in diagnosing GPS, as it often overlaps with other conditions such as irritable bowel syndrome.
Example: A patient is diagnosed with GPS after their doctor rules out other potential causes of their symptoms and observes characteristic patterns in their medical history and physical exam findings.
Chapter 4: Treatment
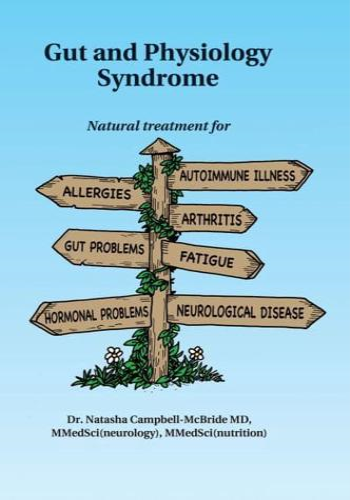
* Reviews the various treatment options for GPS, including dietary modifications, probiotics, prebiotics, and medications.
* Discusses the evidence for the efficacy of each treatment approach and provides guidance on personalized treatment plans.
Example: A patient with GPS is recommended a low-FODMAP diet, which eliminates certain types of fermentable carbohydrates, to reduce symptoms of abdominal pain and bloating.
Chapter 5: Management
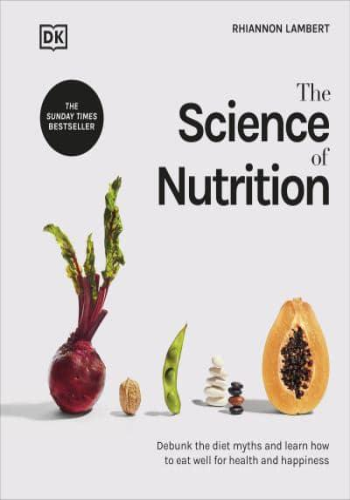
* Emphasizes the importance of lifestyle modifications and self-care measures in managing GPS.
* Discusses stress management techniques, exercise, and sleep hygiene recommendations that can help improve symptoms.
Example: A patient with GPS is advised to practice mindfulness meditation, which has been shown to reduce stress levels and improve overall well-being.
Chapter 6: Prognosis and Outlook
* Provides an overview of the prognosis and long-term outcomes for individuals with GPS.
* Discusses factors that can influence the course of the condition and emphasizes the importance of ongoing management and support.
Example: A patient with GPS who adheres to dietary and lifestyle recommendations experiences significant improvement in their symptoms over time, leading to an improved quality of life.
Chapter 7: Emerging Research and Future Directions
* Examines ongoing research and emerging therapies for GPS.
* Discusses the potential role of fecal microbiota transplantation, novel dietary interventions, and targeted medications in improving patient outcomes.
Example: A clinical trial investigates the use of a specific probiotic strain in patients with GPS, demonstrating promising results in reducing abdominal pain and improving overall well-being.